What Is Claims Audit and Review Management?
In today's landscape of increasing regulatory scrutiny and financial pressures, organizations in the insurance and healthcare sectors are focusing more on claims audit and review management.
This process not only helps ensure compliance but also improves overall operational efficiency.
TL;DR
- Claims audit and review management ensures insurance and healthcare claims are accurate, compliant, and aligned with policies, reducing errors and fraud.
- The process involves selecting claims, reviewing documentation, analyzing findings, and implementing corrective actions to optimize financial and operational performance.
- SmartSuite enhances efficiency through workflow automation, real-time analytics, and AI-driven insights, improving audit accuracy and enabling continuous process improvement.
The Basics of Claims Audit and Review Management
Claims audit and review management involve evaluating insurance claims to ensure they align with policy terms, regulatory compliance, and accuracy in billing. It's a crucial process that forms the backbone of effective financial management within insurance companies and healthcare providers.
Claims Auditing: This is a systematic approach to examining claims data to verify accuracy, prevent errors, and identify areas for improvement. The audit focuses on detecting fraud, managing risk, and safeguarding against financial losses.
Claims Review: While auditing is more about compliance and accuracy, claim reviews are about assessing the necessity and efficiency of claims. This process ensures that services billed are covered and align with contractual agreements and treatment protocols.
The Importance of Claims Audit and Review Management
Ensuring Compliance and Reducing Legal Issues
One of the primary reasons for conducting claims audits is to ensure compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and other industry standards. Failure to comply with these can result in legal issues and heavy fines.
Enhancing Financial Performance
Accurate claims audits help in identifying overpayments and underpayments, thus optimizing financial performance. Organizations can address and recover incorrect disbursements, directly impacting their bottom line.
Fraud Detection and Risk Management
According to the National Health Care Anti-Fraud Association, healthcare fraud costs the U.S. tens of billions of dollars annually. Claims audit and review processes are critical in identifying fraudulent activities and mitigating associated risks.
The Process of Claims Audit and Review
Step 1: Selection of Claims for Review
The first step involves selecting claims that will undergo auditing. This selection can be random or based on specific criteria such as high-value claims or claims from particular providers.
Step 2: Reviewing Claims Documentation and Data
Auditors evaluate claims against policy documents and the patient’s recorded data. This involves scrutinizing billing codes, treatment provided, and the justifications for the claims made.
Step 3: Analysis of Findings
This stage includes analyzing the data collected during the audit to identify trends, areas of high risk, or recurrent issues. This process is essential in developing strategies to address systemic issues.
Step 4: Reporting and Action Plan
Findings are compiled into a report that provides actionable insights. Organizations can then adopt corrective measures such as revising policy terms or employee training programs based on these insights.
Technology in Claims Audit and Review
Claims Management Software
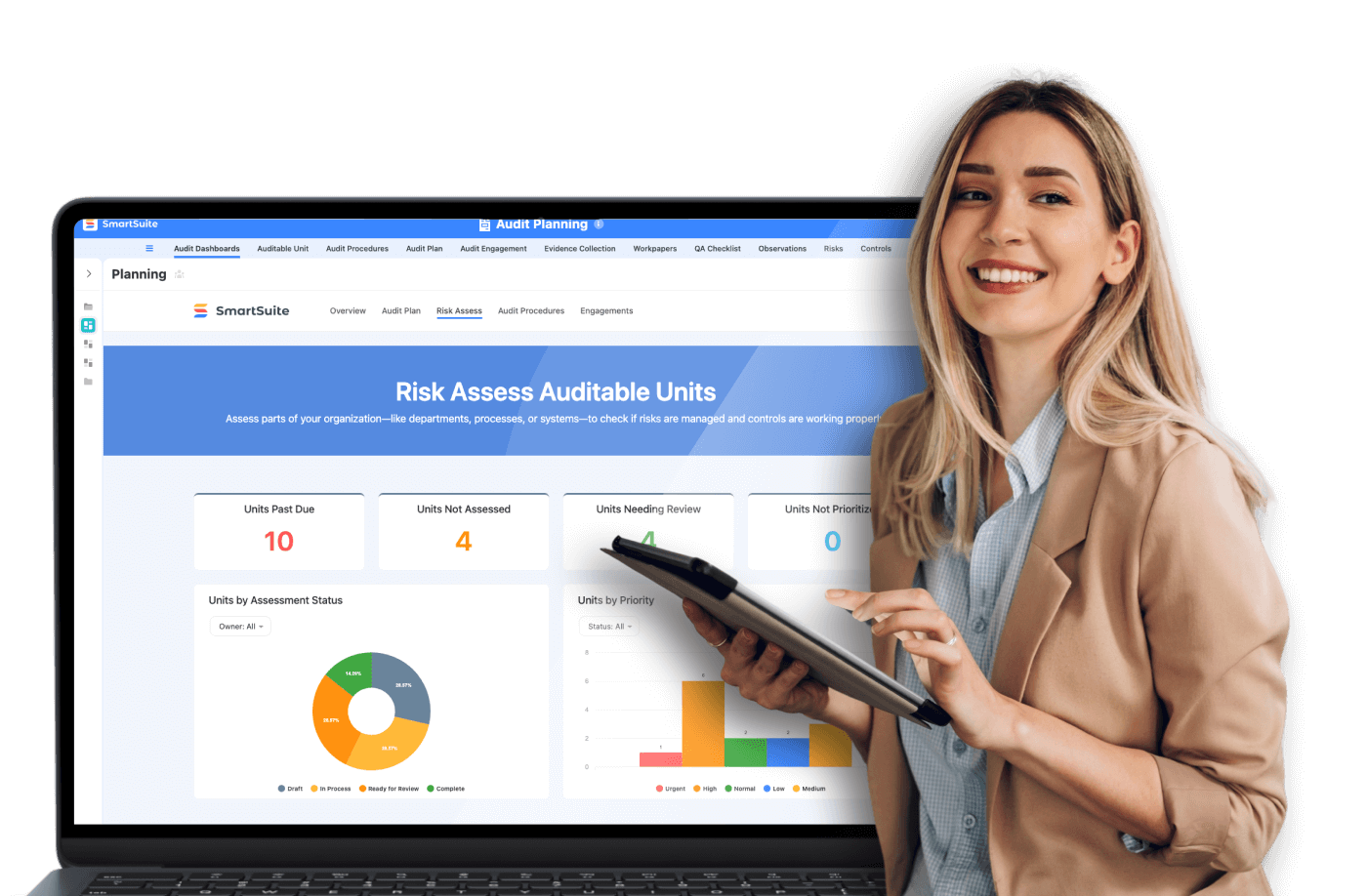
Technological advancements have introduced sophisticated software solutions that facilitate efficient claims audit processes. Platforms like SmartSuite offer integrated capabilities that streamline workflows, enhance data accuracy, and provide real-time insights into claims processing.
Artificial Intelligence and Machine Learning
AI and ML have revolutionized claims audits by automating routine tasks and identifying patterns indicative of fraudulent claims. These technologies significantly enhance accuracy and reduce the time required for thorough auditing and reviewing.
Real-Life Example: Improving Efficiency with SmartSuite
Consider an insurance company that was struggling with delayed audits leading to financial losses. By integrating SmartSuite into their workflow, the company achieved a 40% increase in audit efficiency. The platform's automation tools minimized manual errors, and its real-time analytics provided actionable insights that optimized claims management.
Best Practices for Effective Claims Audit and Review
Implement Regular Training
Staying updated with the latest regulations and audit methodologies is crucial. Regular training sessions for employees can help enhance their skills and knowledge about the claims process.
Maintain Robust Documentation
Documentation should be thorough and easily accessible. This ensures that all necessary data is available during audits, thereby increasing accuracy and efficiency.
Utilize Data Analytics
Employing advanced data analytics can identify trends and potential areas of concern. Insurers can make data-driven decisions to refine their claims processes.
Continuous Improvement Strategies
An ongoing review of audit processes should be in place to foster continuous improvement. Feedback loops, when integrated into claims management systems, can help uncover insights, allowing insurers to adjust their strategies accordingly.
The Future of Claims Audit and Review Management
Embracing Digital Transformation
The claims auditing landscape is rapidly evolving with digital transformation. Insurers willing to embrace these changes can expect improved operational efficiency and reduced costs related to claims management.
Geared Towards Predictive Analysis
Future trends are moving towards predictive analytics, where data-driven forecasts can help preempt compliance issues and claims fraud before they occur.
Conclusion
Claims audit and review management are indispensable in today's complex insurance and healthcare environments. By employing strategic auditing practices and utilizing state-of-the-art technology, organizations can not only ensure regulatory compliance but also significantly enhance their operational efficiency and financial performance. As the industry evolves, the integration of platforms like SmartSuite can be pivotal in advancing claims management and sustaining competitive advantage.
Insurers and healthcare providers are encouraged to assess their current claims processes and consider adopting innovative solutions that bolster their audit and review capabilities. This proactive approach not only minimizes risks and losses but also promotes trust and transparency with stakeholders.
Get started with SmartSuite Governance, Risk, and Compliance
Manage risk and resilience in real time with ServiceNow.



